Surgical Instrument Protection Starts at the Decontamination Sink
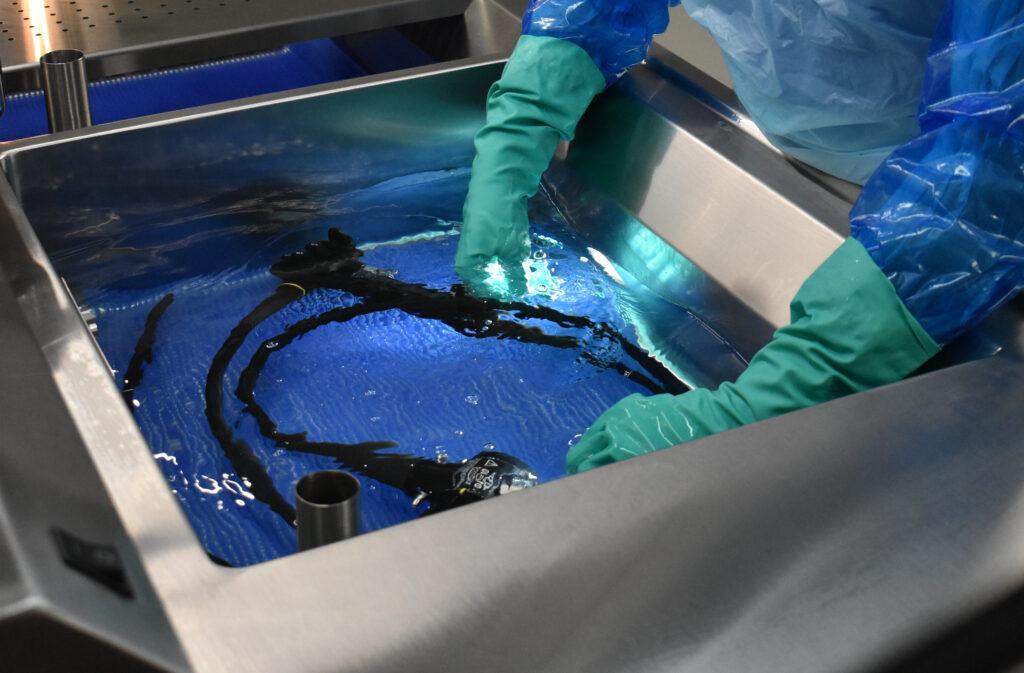
When protecting surgical instruments, many think about the prep and pack area or the case cart. One overlooked area? The decontamination sink.
This early step in the reprocessing cycle lays the groundwork for instrument longevity, patient safety, and overall workflow efficiency.
Why start at the decontamination sink
The decontamination sink serves as more than just an early tool in the reprocessing cycle, it’s the place where frontline defense against bioburden buildup, corrosion, and mechanical damage happens. Instruments arrive from the OR at their most soiled state: exposed to blood, debris, and moisture that, if not addressed promptly and properly, causes irreversible harm.
Improper soaking, poor handling, or insufficient flushing at the decontamination sink often leads to 4 big instrument issues.
1. Corrosion and pitting
Surgical instruments are often made from high-grade stainless steel, which is resistant, but not immune, to corrosion. Extended exposure to blood, saline, or other corrosive fluids, especially without prompt and thorough cleaning, can cause the instrument’s protective passivation layer to break down. This leads to rust, pitting, and irreversible surface damage. Once this occurs, instruments may harbor bacteria in microscopic crevices and require removal from service or costly repair.
2. Stuck or stiff joints
Hinged and ratcheted instruments are particularly vulnerable to build-up in crevices. If joints are not flushed and soaked properly, organic debris and dried soils can accumulate in these small spaces. Over time, this results in stiff movement or complete joint failure, jeopardizing instrument function and risking procedural delays or complications in the OR.
3. Retained bioburden
Ineffective flushing of lumens and cannulated instruments, or inadequate scrubbing and soaking of complex devices, can allow microscopic debris to remain. Retained bioburden poses a serious infection risk and can compromise the efficacy of subsequent disinfection or sterilization. This is especially dangerous in minimally invasive or robotic procedures, where precision tools are reused across multiple cases.
4. Premature instrument failure
The combined effects of mechanical damage, corrosion, and retained debris accelerate the wear and tear on surgical instruments. When instruments fail sooner than expected, departments face increased repair or replacement costs. This can also strain budgets, delay case readiness, and reduce the availability of backup instruments, especially in high-volume ORs.
These issues affect surgical outcomes and result in costly repairs or replacements.
How Decontamination Sinks Support Instrument Integrity
A well-designed decontamination sink plays a critical role in protecting surgical instruments and supporting technician performance. Features such as adjustable height settings, integrated flushing systems, and defined soaking zones clean instruments thoroughly while complying with IFU requirements.
Look for decontamination sinks that offer 5 features which prolong instrument integrity.
1. Instrument-safe soaking areas
Designated soaking zones with clear boundaries prevent instruments from piling up or crowding in one basin. These areas should be sized and shaped to allow full immersion of instruments without stacking, which minimizes the risk of mechanical damage.
2. Hands-free flushing systems
Automated flushing systems provide a safer, more ergonomic method for cleaning lumened and cannulated devices. Thorough flushing eliminates retained bioburden and removes blood and saline residues that can corrode internal surfaces. Effective flushing also reaches tight joints, preventing buildup that causes stiffness.
3. Enhanced visibility and ergonomic support
Integrated lighting such as in-basin or overhead task lights improves visibility during cleaning, helping technicians
inspect joints, hinges, and surfaces more thoroughly. Clearer views support more effective brushing, early detection of damage, and better debris removal while reducing eye strain and improving workflow accuracy.
4. Dedicated timers and compliance tools
Built-in digital timers or soaking countdowns can be essential for meeting the strict time frames outlined in instrument IFUs, especially for enzymatic pre-treatment or manual soak times. Timers remove the guesswork and reduce the risk of under- or over-soaking, both of which can compromise cleaning effectiveness or damage instruments with extended exposure to certain detergents.
5. Silicone liner
Durable, medical-grade silicone liners placed inside sink basins or on staging areas provide a cushioned surface that absorbs impact wheninstruments are dropped or placed quickly. These liners help prevent tip damage, misalignment, and other mechanical stress while also protecting delicate instruments from scratches that could lead to corrosion.
Build a culture of instrument protection, starting at the decontamination sink
Sterile processing departments that prioritize best practices take a proactive approach to instrument safety, starting at the decontamination sink to set the tone for the rest of the reprocessing cycle. Prioritizing this essential step helps reduce repair costs, eliminate workflow delays, and gives surgical teams confidence in the tools they use.
While proper point-of-use treatment in the OR is the first defense in protecting surgical instruments, true reprocessing begins at the decontamination sink, where thorough cleaning and handling practices help preserve instrument integrity and support surgical success.
Interested in learning about our solutions for sterile processing decontamination sinks?
Contact us today to explore solutions tailored to your team’s needs.