The Importance of Best Flushing Practices When Reprocessing Flexible and Rigid Scopes
Properly reprocessing flexible and rigid endoscopes is a critical element of the healthcare infection control process, and following best practices is pivotal. Scott R. Lucas, PhD, PE, program manager, engineering, of ECRI Institute’s AFI Group says, “Hospitals should be diligent in addressing risks related to endoscope reprocessing before a contamination—or even worse, a patient infection—occurs.” The ECRI Institute in 2010 identified cross contamination from flexible endoscopes as number one in the top ten medical technology hazards.
Flexible endoscopy, while common, is subject to high infection control risk. Infection can occur in three ways:1
- Patient to patient
- Environment to patient
- Organisms within the patient’s body
Clinical studies have found reusable endoscope infection risk to be linked to micro-organisms clinging to endoscope biomaterial surfaces. Biofilms are then formed, which often remain wet after processing, and lead to contamination risk. “The formation of endoscopic biofilm during clinical practice can be related to reuse of detergent, manual cleaning, and incomplete drying of processed endoscopes. Developed biofilms protect the micro-organisms from exposure to detergents and germicides, which increase the likelihood of survival through a decontamination process.”2
Diligence to guidelines and manufacturer’s instructions for use (IFU) during scope pre-cleaning will remove the bulk of biobu
rden after endoscope use. But thorough flushing and brushing before any disinfection procedure is required to complete the job. It’s a task that your reprocessing department performs often, considering that a single scope averages 300 to 1,200 uses per year.
Many departments have slightly different manual cleaning protocols for flushing due to the differences in flexible and rigid scopes. It is, however, one of the most critical steps to ensure complete removal of bioburden prior to high level disinfection. It’s helpful if your department has one manual cleaning tool that can meet IFUs for your full scope inventory.
Reducing infection risks with proper scope cleaning protocols
Rigid and flexible endoscopes should be wiped down immediately after use and kept moist. Then the scopes are placed in an enzymatic detergent solution. All channels should be brushed and aspirated during manual cleaning. The channels should then be flushed with detergent. These steps should be performed even on channels not used during the endoscopic procedure. Removable parts are cleaned separately.
Manual cleaning should include brushing and flushing channels and ports according to the manufacturer’s IFU. Using warm tap water for deep cleaning and a disinfectant-detergent solution is standard. Be sure to flush away all disinfectants after cleaning, as they can cause deterioration to delicate instrumentation over time. These areas can become susceptible to hidden microorganisms and pathogens that can infect the next patient. It is important for staff to handle endoscopes with care to avoid excessive coiling or twisting, stacking, or buckling.

Cleaning will require multiple steps and use up to two sinks (preferably three):
- Sink 1: Soak in cleaning solution
- Sink 2: Rinse
- Sink 3: Treated water rinse
Determining the best endoscope flushing solution for your department
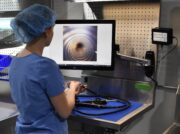
Staff must be as efficient as possible to process a high volume of endoscopes. Staff must also be meticulous in performing scope processing tasks to ensure compliance to cleaning protocols. That’s when having one solution to manually clean different types of scopes and meets compliance, makes a difference. The manual cleaning steps prior to high level disinfection must be thorough and meet IFU and guidelines.
If you don’t already have an ideal single endoscope flushing device solution in your department, you’ll want to look for the following:
- Works with flexible and rigid scopes
- Has the proper adapters for flexible and rigid scopes
- Reduces exposure to chemicals
- Reduces ergonomic impacts to technicians
- Offers an automatic flushing option to run independently
- A pressure relief valve to protect delicate scope channels is compatible with multiple scope channel diameters and sizes
- Can flush cleaning and rinse solutions
Identifying a solution to best fit your department needs, follow IFU, and protect staff from injury is ideal. A proper manual cleaning flushing device should do all of the above and can enable your team to manage a high volume of endoscope processing while achieving staff and, ultimately, patient safety.
Learn more about the FlexiPump’s endoscopic cleaning capabilities, how it can improve staff ergonomics, and automate manual flushing.
Have a problem you’d like help tackling? Let us know!
References:
- Crowson, Carol (2000). Cleaning and disinfecting flexible endoscopes. Nursing Times.
Vol: 96, issue: 38. - Omidbakhsh, N. et al (2021). Flexible gastrointestinal endoscope processing challenges, current issues and future perspectives. The Journal of Hospital Infection. Volume 110, P133-138, April 01, 2021.
- ANSI/AAMI ST91:2021: ANSI AAMI ST91 | Flexible and semi-rigid endoscope processing | AAMI
- ANSI/AAMI ST79:2017: ANSI AAMI ST79 2017 | AAMI