
When One-Size Doesn’t Fit All
Standardization is a highly sought-after goal: it provides consistency around expectations, practices and outcomes. It’s a common goal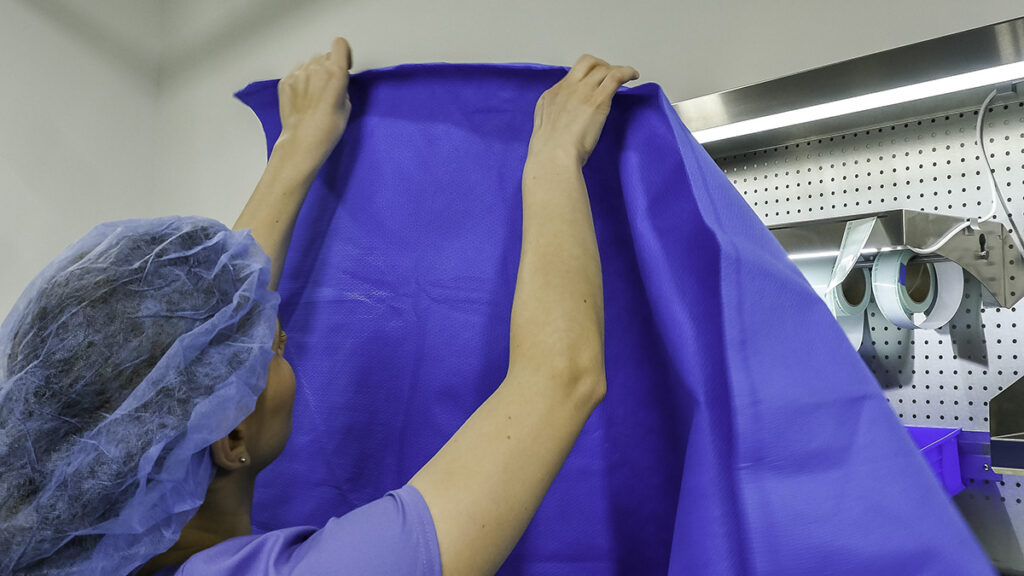 across healthcare, from clinical standards to health system enterprises. The intent behind standardization is to improve quality, optimize available resources and reduce preventable errors. However, are there situations where maybe the opposite can occur in standardization? When standardization overlooks nuances resulting in errors, inconsistencies and glossing over specific steps? Standardization can then have a negative effect on our goals.
across healthcare, from clinical standards to health system enterprises. The intent behind standardization is to improve quality, optimize available resources and reduce preventable errors. However, are there situations where maybe the opposite can occur in standardization? When standardization overlooks nuances resulting in errors, inconsistencies and glossing over specific steps? Standardization can then have a negative effect on our goals.
In sterile processing and endoscope-reprocessing departments, standardization initiatives can take on complex meaning when we acknowledge that not all workflows lead to the same outcomes. There are times where nuance plays a critical role in compliance and safety.
Thinking out of the box, we ask the question: would we get a higher return on investments with a specialized workstation than to ‘cookie-cutter’ our way to compliance?
So where does nuance and standardization intersect?
Specialized Processes vs Standardized Workstations
Start thinking of aspects during reprocessing where processes stand out from the norm. There are unique tasks that pop up through the day that require different resources to get the job done. It can include specialized sizes of wrap or peel packs that aren’t normally stocked at a standardized workstation. It can also be the use of a borescope or other quality assurance measure that requires availability for multiple users over the course of a shift, so placing it at a standard workstation reduces its accessibility to the entire department.
A standardized practice may result in specialized work environments in order to ensure its availability and capitalize on available resources.
High Volume Processes
Is there a process you do consistently enough where having specific resources readily available would aid in the throughput? Circumstances where this can be identified can be if you experience a high volume of low-temperature sterilized medical devices where it warrants having a separate setup, like a wrap table or peel-pack workstation. It provides a new way to organize processes and supplies.
Another example would be instrument types that have separate processes than generalized instrumentation. Examples include ocular instrumentation, laparoscopic and robotic instrumentation or loaner instrumentation. All instrument types where policies and processes vary slightly but enough to call for workflow adjustments to eliminate guess work and misinterpretation of requirements for that specific process. Reducing the number of supplies in one location can help mitigate risk of inadvertent mistakes like the use of incorrect indicators, tapes or labels.
High volume, unique processes can overrun standard work areas and create workarounds, or the constant need to reorganize and rearrange to accommodate the changing needs throughout the day.
IFU and Process Compliance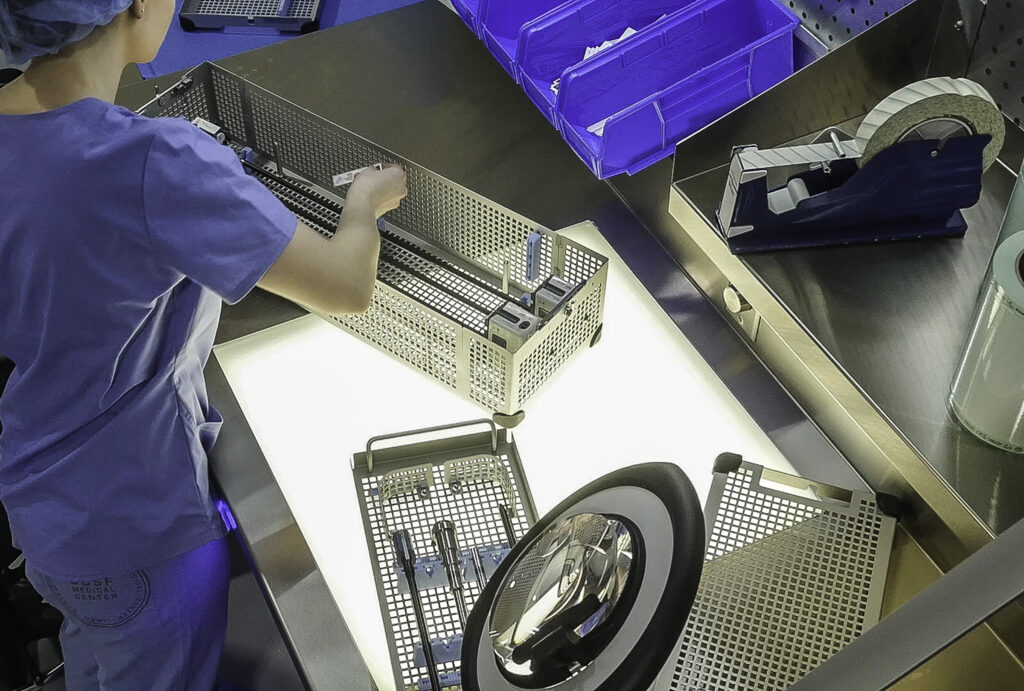
Not all instructions for use (IFU) are created standard; inspection points, tools and steps vary widely. Additionally, the type of instruments we reprocess can increase the number of times a specific task is repeated throughout the day to ensure compliance down to the most nuanced practices.
Where would something like this occur? Loaner trays. Loaner trays come in for a specific time and purpose. Bringing in these sets can require steps to be repeated such as wrapping, traying, weighing and additional data entry that is typically pre-built in our tracking system for owned instrumentation.
These processes can increase the amount of time it takes to process these trays and if supplies and resources are not centralized to a specific location, increase travel and wait time for technicians in an already extended process.
Budget Constraints and Limited Use Case
On the flip side of high-volume case needs, is the limited use case of some tools and inspection equipment. The use of a borescope may be required for certain medical devices being reprocessed, but there isn’t a justifiable volume to justify incorporating it into every workstation in the sterile processing department. Placing a single borescope at a multi-use workstation can limit its availability for use throughout the day and lead to workarounds, and interruptions in order to maintain compliance.
Standardization requires creative thinking, and an understanding that the focus of standardized care is on the outcome, and less on creating a one-size-fits-all process. There is a place for nuance and specialized equipment to ensure all resources are available and at the ready for safe, efficient and quality outcomes.
Curious to learn more about standardization and customization? Check out these links to discover more resources.
https://pure-processing.com/blog/the-weight-of-standardization-the-goal-the-change-and-the-process/
https://pure-processing.com/robotics-implementation-checklist/







