Imagine requiring a surgical procedure on your hip. It’s a standard surgery performed hundreds of thousands of times every year in the US. You don’t spend much time considering that something could go wrong. Now imagine a couple weeks have passed since your surgery. You feel great and have a follow-up appointment with your surgeon. The surgeon confirms you’re healing well, and you are very thankful to the surgeon for a successful procedure and your ongoing recovery.
Unfortunately, some people are not so lucky. Some patients do experience unforeseen and unnecessary consequences from routine procedures, leaving them with a surgical site infection (SSI) or  other healthcare-associated infection (HAI). While you were right to thank your surgeon for doing an excellent job, you also should have thanked the Sterile Processing Department (SPD) for properly cleaning, disinfecting, inspecting, and sterilizing the instruments before they were used during your procedure. The risk of an SSI would have increased if the sterile processing department had not properly cleaned the instruments used.
other healthcare-associated infection (HAI). While you were right to thank your surgeon for doing an excellent job, you also should have thanked the Sterile Processing Department (SPD) for properly cleaning, disinfecting, inspecting, and sterilizing the instruments before they were used during your procedure. The risk of an SSI would have increased if the sterile processing department had not properly cleaned the instruments used.
Two types of healthcare-related infections
What are healthcare-associated infections and surgical site infections?
- An SSI is an infection that occurs after surgery in the part of the body where the surgery took place. While they are both infections resulting from medical treatment, SSIs refer specifically to an infection acquired in surgery.2
- HAI’s are infections acquired while receiving any treatment, not only in surgery.
According to the CDC, “each day, approximately one in 31 U.S. patients contracts at least one infection in association with his or her hospital care”.1 That number might seem high, but it would certainly be higher if the central sterile department wasn’t doing its job properly.
How sterile processing prevents infection
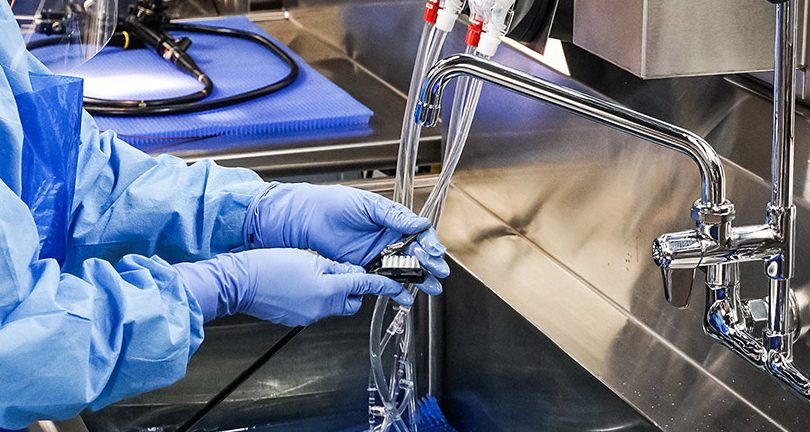
What role does SPD play in preventing these infections? When instruments are used between patients, residual human bio-burden on surgical instruments (blood, feces, mucous, bone, etc.) can potentially contaminate another patient. Sterile processing follows strict, technical instructions for use (IFU) to ensure every crevice, corner, hinge, bend, and channel of medical instruments are thoroughly cleaned. Instruments must also be fully functional. Surgeons can potentially make unnecessary mistakes during the procedure if scissors get stuck, if blades don’t cut, and graspers can’t grasp.
Sterile processing departments need highly technical and efficient devices to perform their job correctly. For example, even a department’s reprocessing sink should be considered. If a sink can’t fit the large, heavy instruments used during a hip surgery, how can they be properly cleaned? These sinks are not just sinks you would find in your house or a restaurant, nor are the brushes, sponges, detergents, washers, and other pieces of specialized equipment. Because SSIs, HAI’s, and patient safety are such serious concerns, they need to be treated as such with the proper equipment.
The sterile processing department in your hospital is crucial to patient safety and is needed to run a safe, efficient, and effective surgical department. So next time, if ever, you need to go in for a surgery, make sure to not only thank the doctors, surgeons, and nurses, but also the people working behind the scenes to keep you safe: the sterile processing department.
Looking for more information on improving cleaning outcomes to prevent surgical site infections and HAI’s? Watch our free, 1 CE program, A Royal Flush: Your Winning Hand for Pre-Cleaning Protocol, to learn how the reprocessing sink is at the heart of every successful patient procedure.
References
- “Current HAI Progress Report.” Centers for Disease Control and Prevention, Centers for Disease Control and Prevention, 26 Oct. 2021, https://www.cdc.gov/hai/data/portal/progress-report.html
- “Surgical Site Infection (SSI).” Centers for Disease Control and Prevention, Centers for Disease Control and Prevention, 24 Nov. 2010, https://www.cdc.gov/hai/ssi/ssi.html




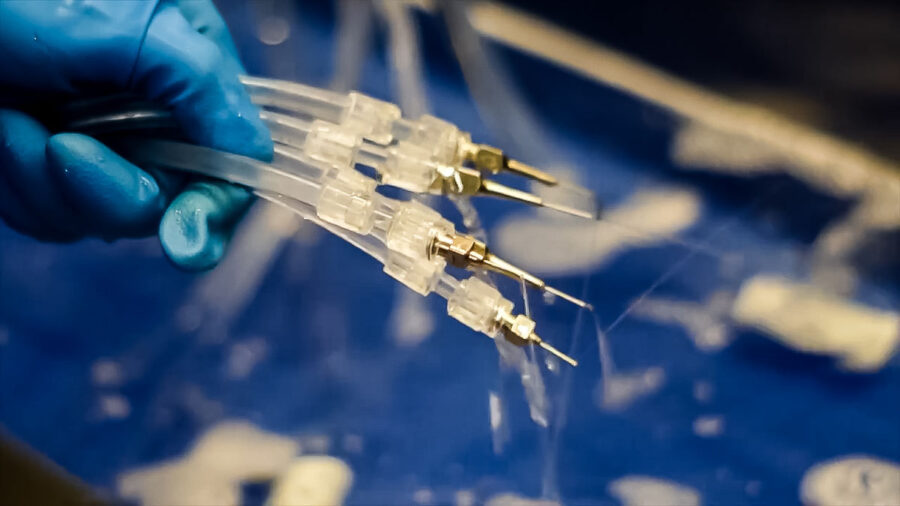
 instrumentation fully to deliver high quality cleaning outcomes. External inspection is good for 50% of the device, but what about the other half of your instruments? The internal channels and components of devices are as important and yet more dangerous to leave unchecked.
instrumentation fully to deliver high quality cleaning outcomes. External inspection is good for 50% of the device, but what about the other half of your instruments? The internal channels and components of devices are as important and yet more dangerous to leave unchecked. It’s impossible to ignore. Instrument reprocessing time has increased. A major factor? Extended instrument soaking.
It’s impossible to ignore. Instrument reprocessing time has increased. A major factor? Extended instrument soaking.