From the sterile processing technician on the front lines, the manager keeping the workflows running, the educator making sure everyone is trained, to the director advocating for resources and guiding departments across campuses, every level of sterile processing has a unique and important impact on patient outcomes.
One SPD Director, Kenneth Campbell at Berkshire Medical Center in Pittsfield, MA, offered to share his perspective on his role in sterile processing services. Campbell has an extensive history in central sterile. Beginning at the age of 17 he enlisted in the armed services as a surgical tech, and grew into his role today as Director of SPD, member of the HSPA Board of Directors, author of Time to Talk… What They Didn’t Tell Me, and host of the Time to Talk podcast. His passion for the sterile processing industry is self-evident, and contagious.
As Director, Campbell shared his many insights and perspectives in his role.
The Importance of SPD
Campbell expressed great emphasis on the importance of sterile processing departments, and with good reason. Without sterile processing departments doing their job, doctors and nurses are unable to adequately do their role, with the patient suffering most.
Conveying the importance of sterile processing is easier said than done. In many facilities, members of the C-Suite view the SPD as nothing more than a department on paper; they have never visited a sterile processing department, aren’t necessarily sure of its role, and don’t have an understanding of what it takes to enable a sterile processing department to operate at its finest.
At Campbell’s facility, however, this is not the case. As Director of SPD, he consistently advocates for members of different teams, including the C-Suite and OR, to come visit his department and get an understanding of the SPD’s functions.
The effort has paid off tremendously. With heightened awareness of SPD’s role, Campbell has been able to not only make improvements within SPD but create a career ladder for members of his team to work their way up to some of the highest SPD pay in the industry.
Evolution of Sterile Processing
“I remember getting deployed and you had you had to literally pour the water in the back of the sterilizer just to do a load versus now, just walking up to it and pushing a button. Yeah, evolution is great.”
During his time in SPD, Campbell has seen wide-ranging changes come to the sterile processing profession. From reservoir-fed sterilizers, to biologicals going from three hours to twenty minutes, many improvements have been realized in the space.
Equipment isn’t the only aspect of SPD that’s evolved; best practices have evolved significantly over the years as well. Campbell points to standardization being the most substantial influence on that evolution, and recalled the way it used to be:
“I’ve taken over facilities where it was common practice in the OR if something went down or dropped or whatever it was, somebody went to a common sink and ran it, rinsed it off, and threw it inside of a flash pan and went back to the OR with it. That is not the best practice by far, but back when that was the norm, nobody said anything. Infection rates weren’t a thing that people kept an eye on.”
Standardization has given educators, managers, and directors the tools necessary to help ensure their team contributes to an environment of patient safety at every level, but that doesn’t necessarily mean the standards have been universally adopted the way they’re meant to be.
Current Challenges
“[Standardization] is still a challenge to this day. I can sit here and say all day long that we trained to the standard, right? You train somebody to the standard. They know all of the steps, but you could walk into any decon, any prep & pack area in America, and you’re going to find somebody doing something different, even though we know what the book says. Getting people to all follow  the same thing. It’s probably our biggest challenge.”
the same thing. It’s probably our biggest challenge.”
While Campbell praises the guidelines and standards that have contributed to enormous boosts in patient safety and central sterile processes, the ability of departments to keep up with and adhere to them is something he considers to be a growing problem.
“I had to buy new sinks because the standard says we should be using the three-sink method. But based on how some facilities were built way, way, way before that standard, they can only fit two sinks. How can we hold somebody to a standard that doesn’t or can’t exist in their facility?”
A significant limiting factor for many departments is the cost associated with equipment that meets recommendations and requirements; many SPDs don’t have large budgets to begin with, and the problem is amplified if those setting the budgets don’t have an appreciation or understanding of what sterile processing is tasked with accomplishing.
“If people don’t see the importance of what sterile processing does, not everyone is going to be willing to give up those budget dollars.”
Advice to Future SPD Directors
If you’re interested in SPD leadership and being a Director of SPD, Campbell offered one piece of advice: Never stop being a tech.
“If you lose touch of that inner tech and then you become corporate, you will lose your staff. You will lose the confidence of your people. And then there’s nothing you can do to get that back.”
Campbell also offered advice related to developing the leadership qualities needed to be a successful Director of SPD, including:
- Listening: always listen to what’s being said in your department and learning from it.
- Never stop improving: take steps using what you learn to find ways to continually improve yourself.
- Bring people with you: leadership requires elevating other people and helping them achieve their goals. Be the person in your department that wants to see everyone succeed.
- Mentor: share what you’ve learned with others and help them navigate sterile processing with the knowledge you’ve gained during your time.
Campbell also put emphasis on the fact that career progression does not happen overnight. A lot of work needs to be done to gain the technical, managerial, and leadership skills necessary for success.
Further, professionalism is important to keep in mind from the get-go. If your goal is to achieve a leadership position within your department, the way that you act and treat people will play a significant role in your ability to lead later in your career. When your peers become your direct reports, the nature of your relationship changes, and it’s difficult for the former “class clown” to begin having difficult conversations and keeping the department on the right track.
Conclusion
SPD Directors fill many roles. They’re the advocates for their department internally and externally. They make sure the right people are in the right position. They develop employees and form the next generation of leaders. Most importantly, they work tirelessly to ensure their departments are doing everything possible to deliver the safest conditions for patients.
It’s clear that Kenneth Campbell’s passion for the industry runs deep, which is exactly what you want to see from a Director of SPD.
Interested in other perspectives from SPD? Check out these other blog posts:
Traveling SPD Manager
Educator
About: Perspectives
Perspectives is a series of articles written to present a deeper look into the unique profiles, experiences, and backgrounds in the sterile processing community. By evaluating our industry through the unique lenses of its people, we can better understand our impact on each other, our patients, and our communities. Thank you to those who offered their time to write these articles with us. We appreciate your time, and your commitment to your patients and staff!

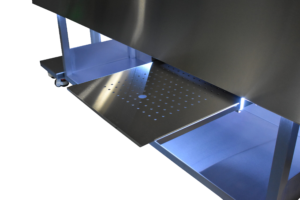
 endoscopes. Automated flushing systems make flushing scopes much easier, while eliminating a painful repetitive motion that has the potential to lead to carpal tunnel complaints.
endoscopes. Automated flushing systems make flushing scopes much easier, while eliminating a painful repetitive motion that has the potential to lead to carpal tunnel complaints.







 their set up to ensure compliance.
their set up to ensure compliance.
 cognitive and physical ergonomics, customization allows for the consideration of the employees and their unique interactions with their job and the standards & regulations that are imparted on them to adhere to.
cognitive and physical ergonomics, customization allows for the consideration of the employees and their unique interactions with their job and the standards & regulations that are imparted on them to adhere to.



 the same thing. It’s probably our biggest challenge.”
the same thing. It’s probably our biggest challenge.”





