In August, we brought our Voice of the Customer panel together to delve into a topic that SPD professionals across country identified as top-of-mind in our 2023 SPD State of the Industry Report: training and education.
One of the most challenging aspects of addressing training and education concerns in sterile processing is acquiring the resources to provide to your team.
We collaborated with Gene Ricupito, Sr. Project Manager, Sterile Processing at University of California San Franscisco (UCSF) to dive deeper into this topic.
Determining what resources to use
Figuring out what resources you want to use to achieve your training and educational goals can be tricky. . An abundance of material is available to choose from or create. The first action Gene takes is conducting an assessment to determine general competency of his team.
“Does it tell me I have a high performing, low performing, or average performance workforce. That’s going to inform how rapidly I need to take action.”
With an understanding of your team’s competency understood, the next step is to incorporate your department’s larger strategic goals to ensure that the training and educational tools you deploy develop your team in support of achieving those goals.
“It’s like that old saying about skating to where the puck is going to be, not where it is right now.” Gene explained.
Ricupito recommends creating a 2–3-year training and education plan that informs the resources you’ll deploy. A few examples to consider:
- “Our department is expected to grow significantly, I need to make sure I’m giving key team members the ability to develop leadership and management skills.”
- “We’ll be taking over scope reprocessing after this project is completed, it’s important to get a few teammates trained up on scopes.”
- “The facility’s robotics volume is expected to go up this year, the newer members of my team would benefit from additional in-servicing to make sure we can keep up.”
As you identify the goals of your department, you can determine which resources will best serve your team’s needs.
The most valuable training and educational resources
Most departments have a mix of resources they leverage for training and education. Ricupito and our VOC panel identified the resources that they consider to be most valuable to include:
- Source materials: Having the source materials, such as print and digital versions of ANSI/AAMI standards, Joint Commission requirements, as well as manufacturer’s Instructions for Use (IFU) for equipment and instruments can help teams easily reference and reinforce their knowledge of them.
- Vendor-created resources: Vendors have created and made many digital videos and courses available. These are some of the most popular, especially in departments without dedicated educators.
- In-services: Ricupito emphasized that the most impactful way to keep teams trained on instrumentation and equipment is to have vendors come onsite for in-person in-services. This allows teams to ask questions and get clarity.
- Physical/Hands-on workshops: Allowing teams to handle and learn about equipment and instruments in a no-pressure environment helps them familiarize themselves better when they’re not pressed for time.
Creating training and educational content in-house
There are many benefits associated with departments creating training and educational content on their own:
- Laser focused: When developing your own training and educational resources, departments can zero-in on what their department needs. Rather than trying to hunt down several resources that cover a certain topic, educators can create optimized content to meet their department’s unique needs.
- Trim the fat: Content created internally doesn’t contain unnecessary information that may confuse or bog down the person consuming it. In-house educational tools can get straight to the point, reducing the amount of time needed and distilling information into easily digested formats.
- Department-specific: Training resources developed in-house can include department-specific information, such as images, diagrams, SOPs and workflows that are currently in use. This gives them a clearer understanding of how the training and education applies within the department they’re a part of.
Internally-developed central sterile training and educational resources aren’t easy to create. Some barriers to entry are associated with creating content on your own:
- Bandwidth: Creating resources internally requires the bandwidth to do it well. If a department is unable to commit the time to developing valuable, thorough education, they’re probably better off using pre-existing ones.
- Skillset: Educational content creation requires certain subject matter expertise that not all departments will have on their team.
- Investment: Home-grown training materials are costly to develop. From the time an educator spends researching and building content, to the tools necessary to effectively deliver and convey the information needed, many costs contribute to the overall investment.
- Sustainability: Once a department has committed to and executed on developing their own training and educational materials, there’s still work to be done. The resources require regular review and updating to ensure that it’s keeping pace with changes happening in the sterile processing industry.
While the benefits of in-house training and education resources provide significant benefits in terms of focus and effectiveness, those benefits come with a cost that not all departments can accommodate.
Making the case for more resources
Sterile processing budgets are always deliberately allocated; every last dollar is needed, and it’s often not enough. So how can you make a case to increase investment in training and education in your department?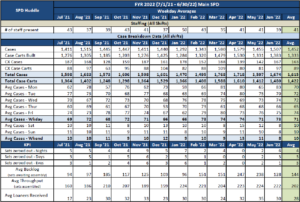
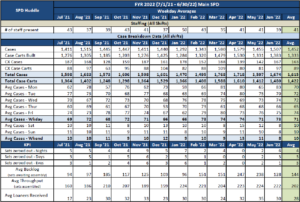
- Show up with data: As Ricupito explains:
“If you’re making a business case [to increase SPD budget for training and education], when you get to the decision maker, you’ve got three bullet points. That’s it, that’s all the attention you’ll get. You’ve got to be able to say ‘If I do X, Y will happen, and here’s the data to prove it.”
- Tell the historical story: Pointing to specific quality outcomes with historical data and a good case for the positive impact of training elevates the discussion from an SPD problem to an organizational problem, adding urgency to resolving it.
- Talk to physicians: Many in SPD can relate to the story of an upset surgeon letting the department know how they feel about a mistake. Ricupito explained that a clearer understanding of SPD by the OR, and vice versa, often contributes to mutual support of one another to begin solving problems as a team. If SPD is able to demonstrate the source of some OR frustration is rooted in a lack of training and education, there becomes an incentive for the OR to advocate for SPD.
Lean on your vendors
“The most successful companies serving sterile processing are the ones that continue educating their customers.”
Training and education is a tricky variable in the sterile processing equation. Most departments need more of it, but many lack the resources or dedicated educators to make it happen on their own. Enter: vendors.
Many vendors have a wide array of training and educational resources available for their customers, free of charge. SPD teams can find free CE’s, videos, guides, on-demand online in-services, and more on a vendor’s website. Further, many vendors want the opportunity to help departments out, whether it’s in the form of a live in-service in your department, or a digital one on a platform like Zoom or Teams.
Lean on your vendors to provide training and educational resources that your department needs; there’s no reason to reinvent the wheel.
Conclusion
Obtaining additional training and educational resources for your department involves many considerations. Once you’ve identified what your department needs, you’ve only just begun the process.
Some sources, such as copies of standards and guidelines for your team, allow passive reference when needed, others, such as in-house content provide immense, focused benefits, if your department has the bandwidth to take something like that on. Making the case for additional money to support training and education can be tough, but if you show up with a plan and data to back it up, you’ll have a much better shot.
External influences have an impact here, too; communicating with your OR counterparts can help shine a light the source of problems they’d like to see resolved just as much as SPD does. Finally, turn to your vendors. Get them scheduled for in-services and look at their websites for training and education opportunities.
Want to get the ball rolling? Explore Pure Processing’s complimentary CE offerings!
About: Voice of the Customer Committee
The Voice of the Customer Committee is a panel of healthcare and instrument reprocessing professionals who have graciously donated their time to share their expertise and guidance on current challenges faced by the instrument reprocessing community. Through sharing their insights, experiences, and best practices, we have been given the opportunity to share these findings with our readership. We’d like to thank our VOC members for their outstanding input and insights, as well as their time! Thank you for your continued partnership, and all you do.






















 tight space allotted for their scope sink, and two windows further constricting the way the space could be used, single basin sinks felt like the only option.
tight space allotted for their scope sink, and two windows further constricting the way the space could be used, single basin sinks felt like the only option.