Standardization. A word widely used in healthcare today to define the goal of consistent and reliable care across the healthcare industry. Having standardized processes, equipment and workflows can lead to greater efficiencies, fewer questions regarding procedures and can open up avenues for “cross-training” of staff to fill in for staffing variances across departments and system wide facilities.
Hospitals go through accreditation processes such as Joint Commission or Nursing Magnet designations to showcase the importance and accountability towards standardized, high-quality care. Sterile processing department’s across the United States reference standards and guidelines, such as ANSI/AAMI and AORN, or manufacturer instructions for use (IFUs) to ensure they are complying with current standard practices and processes to achieve the appropriate and safe outcomes our patients expect.
However, standardization hasn’t come without its fair share of scrutiny and concern including the debate that it can create transactional experiences, discourage autonomy in personalized care and  potentially lead to adverse outcomes as a result. (Sinsky, et al 2021) There are pitfalls and imperfections within any mode of practice, and humans are at risk of falling into a rhythmic, box checking mode. At the core, a strong standardization program is intended to “create efficiencies that generate the additional time needed for personalized care.” (Sinsky, et al 2021)
potentially lead to adverse outcomes as a result. (Sinsky, et al 2021) There are pitfalls and imperfections within any mode of practice, and humans are at risk of falling into a rhythmic, box checking mode. At the core, a strong standardization program is intended to “create efficiencies that generate the additional time needed for personalized care.” (Sinsky, et al 2021)
- For example, flushing with syringes can be a standardized approach to manual cleaning. However, this practice has several variabilities that lead to inconsistent outcomes and approaches including: No user does it the same, and sometimes the same user can do it differently at the start of their day as opposed to the end of the day when fatigue sets in.
- Syringes come in varying sizes
- Both volume and pressure can’t be finely controlled by technicians, especially in a fast-paced environment
Determining what, how and when in standardization can be a tricky endeavor to navigate. A creative way to ensure that our standardization leads to greater efficiency and opens doors to more personalized approaches can be done by working your considerations backwards. Starting with what you want your team to achieve and tracking back to the place of improvement can help determine action items, and account for needed flexibility to ensure accurate and impactful quality of care.
The Goal
Goals are built based on several scenarios or situations. This measure for improvement will originate from things like new standards, identified gaps in practices, or new trends that prove the need for added or updated quality assurance measures.
ANSI/AAMI ST79: 4.3.1 addresses education and standardized work to protect reprocessing professionals from potential hazards, ensures the appropriate education and training are presented to each person, and sets the expectation for safe and appropriate medical device reprocessing.
“Education, training, and standardized work practices decrease the risk of operator error during reprocessing and help ensure that personnel are conversant with the latest data and techniques. Education and training are an important aspect of any program intended to protect employees from a potential safety hazard. Without it, the employee might not recognize unsafe conditions or work practices and might not know how, when, or why to employ protective measures. The health care organization’s policies and procedures are a necessary part of any education and training program, and all personnel should be familiar with and adhere to these policies and procedures. Documentation of education and training is required by accrediting agencies.”
The goal is the desired outcome, such as a determined metric (ie. X number of trays sterilized per day), percentage of accuracy (X% reduction in bioburden findings) or a process upgrade, such as a move from a manual process such as manual flushing, to an automated flushing device.
Setting goals without understanding the nuance of your teams, processes, volumes and current procedures can lead to slow implementation, poor buy-in or work arounds that can impact time and efficiency, at times making more work where the goal was to reduce it.
The Change
Once the goal is determined, it positions change leaders to understand the scope of impact by looking at the reprocessing cycle from start to finish to understand where and what parts of the process will change.
Implementing standardized practices often results in adjusted workflows beyond the single step or process point, or triggers a change in routines, sometimes in start or close-of day routines. For example, if you were to convert to an automated flushing or automated dosing system, it would lead to incremental testing to ensure functionality, which needs to be accounted for in the daily tasks and assignments.
Limiting the view of the goal into a singular process can lead to oversight of time allocation and necessary resources that are required properly integrate standardized processes, losing the opportunity to truly capitalize on its full benefits.
Considering the changes required and being upfront about the adjustments in responsibility are key objectives to address during initial considerations and matching the goal with the proposed standardized practice or product. When these objectives are not analyzed and reviewed against the larger picture of reprocessing as a whole, it can lead to work arounds or gaps either at the front and proceeding steps to follow, resulting in a loss of effectiveness.
The Process
Understanding the goal and the impact it has on the whole of a process from start to finish can pinpoint how to implement the proposed standardization and best prepare for the upcoming changes. This can include understanding learning curves, new resources that will be made available and understanding how it will change the steps in the process.
Processes can look different. For automated flushing, the steps go from individual, single port flushing, to sorting and hooking up multiple lumens and starting the flushing equipment for a pre-determined amount of time and fluid volume. This now changes what happens with the time that was once committed the syringing process.
- What are some new ways to utilize the time originally spent flushing?
- How does the daily maintenance impact the start of your mornings?
- Is there a cost savings? If so, what other opportunities can now be considered with the budget adjustment?
These questions are not punitive, but an opportunity to consider the other side of efficiency which is the additional time and space granted to expand the benefits of standardization.
Standardization, when done correctly, can create autonomy and a personal touch that healthcare calls for where it is most needed. Standardizing work can set appropriate expectations and create opportunities to focus our time, development and energy into the nuanced tasks that require a personal touch and flexibility. Together standardization and personalized care can lead to a more robust quality management system within sterile processing and endoscope reprocessing departments, making processes more intentional and reliable.
Interested in other resources to help you improve your department? Check these out resources out!
Education:
The Cost of Cutting Corners Blog: Earn 0.5 Free CE
Luminosity Requirements in Instrument Reprocessing Blog: Earn 0.5 Free CE
Additional Resources:
Luminosity Compliance Checklist
References
Sinsky CA, Bavafa H, Roberts RG, Beasley JW. Standardization vs Customization: Finding the Right Balance. Ann Fam Med. 2021 Mar-Apr;19(2):171-177. doi: 10.1370/afm.2654. PMID: 33685879; PMCID: PMC7939702.ANSI/AAMI ST79: 2017




 ergonomic support, reducing pressure on the hands and wrists during extended cleaning sessions.
ergonomic support, reducing pressure on the hands and wrists during extended cleaning sessions. minimal effort.
minimal effort.  resolution image provided by borescopes ensures that even the smallest particles are detected, enhancing the thoroughness of inspections and preventing missed contaminants that could lead to reprocessing.
resolution image provided by borescopes ensures that even the smallest particles are detected, enhancing the thoroughness of inspections and preventing missed contaminants that could lead to reprocessing.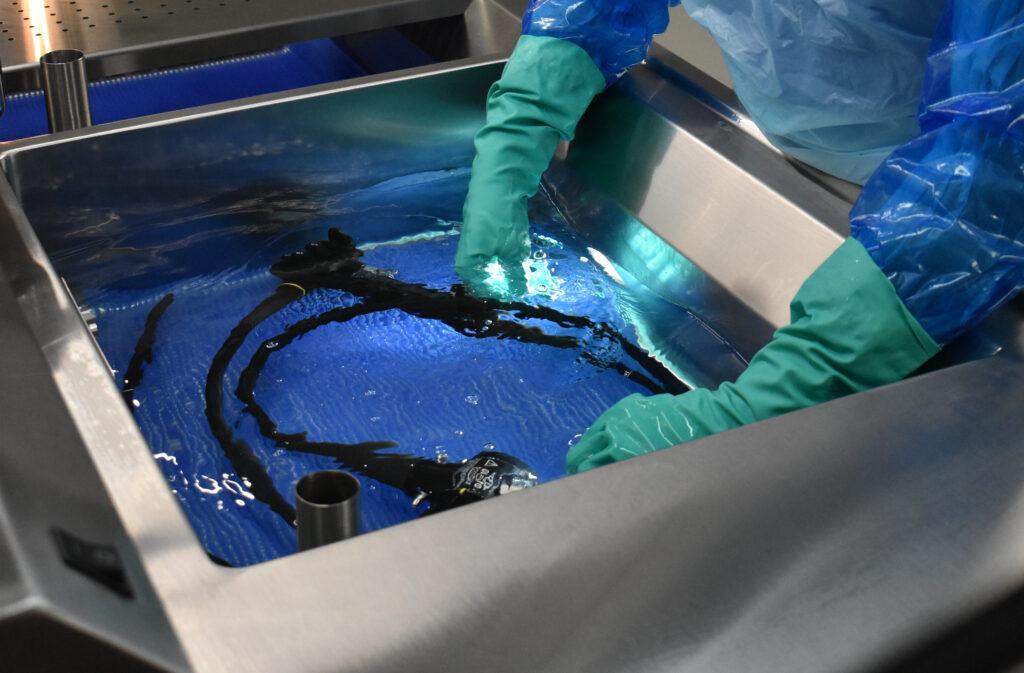 areas.
areas.  under standard lighting conditions. Further, small cracks and crevices in instruments can harbor residue that the human will simply never be able to pinpoint on its own. If these are missed in decontamination, they will need to be sent back and effectively reprocessed twice.
under standard lighting conditions. Further, small cracks and crevices in instruments can harbor residue that the human will simply never be able to pinpoint on its own. If these are missed in decontamination, they will need to be sent back and effectively reprocessed twice.









 will likely play an important role in the training of new teammates, so ensuring they understand newly introduced training policies, pacing, and methods will help them assist and train new hires in a way that’s aligned with your goals.
will likely play an important role in the training of new teammates, so ensuring they understand newly introduced training policies, pacing, and methods will help them assist and train new hires in a way that’s aligned with your goals.



